Pharmacovigilance: A promising approach for better health outcomes
The pharmaceutical industry and drug regulators face numerous challenges in pharmacovigilance, patient safety, and addressing areas of unmet medical needs in an environment where development costs have increased exponentially while filings and launches have decreased significantly.
The confluence of these problems not only intensifies access limitations and costs over time but also generates a pressing need for investments in new, improved PV capabilities. To provide analyses to regulators, healthcare professionals, and patients quickly and transparently, these improved capabilities will enable businesses to improve the processing of safety data.
To improve the accessibility, assessment, and dissemination of the information, it is necessary to review the current PV systems. This fact is causing businesses to work with local, national, and regulatory agencies and healthcare delivery systems to develop a model that will guarantee operational efficiencies and satisfy the needs of doctors, patients, and payers by automating a significant portion of the event reporting and processing.
The status of PV must change to one that benefits the market, regulators, and patients to constitute a true breakthrough. We present a few crucial factors to think about for a thorough PV transformation to realize this paradigm.
Effective collaborations
Up until a circumstance that brings to light drug safety concerns, the tendency has been to keep things as they are. Because of these obligations, the pharmaceutical industry has long regarded PV as a sacred domain whose only goal is the observance of predetermined data collection and reporting requirements. Proper techniques for dealing with new issues and challenges called for solutions that were more involved, complicated, and resource intensive.
An organizational transformation for PV has also been accelerated by changes in the regulatory environment in the US. The traditional method of signal detection and evaluation through existing PV strategies has become an unworkable paradigm due to the need for new adverse event reporting, safety monitoring requirements, and risk management. As a result, the creation of a flexible and effective next-generation PV solution will necessitate not only internal transformational leaps but also creative external partnerships.
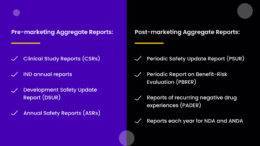
The proactive risk-benefit assessment and timely transactional PV components, such as the receipt and processing of adverse events and the cost-effective creation of aggregate reports, should all be capabilities of the new PV model that is more effective and agile. The extent to which these changes occur will depend on several variables, including advanced technologies, effective means of exchanging safety information, and inspirational leadership that inspires fresh partnerships between various partners and disciplines. These innovative methods will make it easier to move from a discipline that has historically been reactive to a proactive paradigm of viable and effective models intended to continuously improve patient safety.
For risk identification, risk assessment, and risk management, this proactive system depends on external, creative partners. A major focus of improving drug safety systems is ongoing risk-benefit analysis throughout the product life cycle. This is especially true after launch when the ongoing evaluation of risk-benefit is necessary as new data become available. As a result, PV departments will need to actively advance their science by combining existing PV methods with those from epidemiology, health services research, and health economics. By combining various data, scientific disciplines, and methodological expertise, this discipline integration will give PV departments a synergistic advantage in detection and management.
Only through collaboration between businesses, policymakers, academic institutions, and healthcare delivery systems will it be possible to supplement current PV methods with new disciplines.
Increasing patient safety with pharmacovigilance
The pharmaceutical industry and drug regulators face numerous challenges in pharmacovigilance, patient safety, and addressing areas of unmet medical need. There has been a significant decline in filings and launches during this time of exponentially increasing development costs.
Increasing access limitations and costs over time are generated by these problems, as well as a pressing need to invest in better PV technologies. To provide analyses to regulators, healthcare professionals, and patients quickly and transparently, these improved capabilities will enable businesses to improve the processing of safety data.
Reviewing PV systems is necessary to improve the accessibility, assessment, and dissemination of information. This requires businesses to work with local, national, and regulatory agencies and healthcare delivery systems. They will develop a model that will guarantee operational efficiencies and satisfy the needs of doctors, patients, and payers. In addition, they will automate a significant amount of event reporting and processing.
The status of PV must change to one that benefits the market, regulators, and patients to constitute a true breakthrough.
Effective collaboration
Up until a circumstance that brings to light drug safety concerns, the tendency has been to keep things as they are. Because of these obligations, the pharmaceutical industry has long regarded PV as a sacred domain whose only goal is the observance of predetermined data collection and reporting requirements. Techniques are applied to address concerns and challenges that require solutions that are more involved, complicated, and resource intensive.
Organizational transformation for PV has also been accelerated by changes in the regulatory environment in the US. The traditional method of signal detection and evaluation through existing PV strategies has become an unworkable paradigm. This is due to the need to enhance adverse event reporting, safety monitoring requirements, and risk management. As a result, the creation of a flexible and effective next-generation PV solution will necessitate not only internal transformational leaps but also creative external partnerships.
The revised PV model should provide proactive risk-benefit assessment and timely transactional PV components, such as the receipt and processing of adverse events and the cost-effective creation of aggregate reports, which are all capabilities that are more reliable and agile. The extent to which these changes occur will depend on several variables. These variables include advanced technologies, reliable means of exchanging safety information, and inspirational leadership that inspires successful partnerships between various partners and disciplines. These innovative methods will make it easier to move from a discipline that has historically been reactive. This is because they are viable and effective models intended to continuously improve patient safety.
For risk identification, risk assessment, and risk management, this proactive system depends on external, creative partners. A major focus of improving drug safety systems is ongoing risk-benefit analysis throughout the product life cycle. This is especially true after launch when the ongoing evaluation of risk-benefit is necessary as updated data become available. As a result, PV departments will need to actively advance their science by combining existing PV methods with those from epidemiology, health services research, and health economics. By combining various data, scientific disciplines, and methodological expertise, this discipline integration will give PV departments a synergistic advantage in detection and management.
Only through collaboration between businesses, policymakers, academic institutions, and healthcare delivery systems will it be possible to supplement current PV methods with novel disciplines.
Globalization of markets
Cost savings have helped multinational corporations transition from using global sourcing as a trend to largely common practice. Global sourcing, though, offers more benefits than just cost savings. For PV, global sourcing will entail integrating on-site and offshore capabilities as well as creating centres of excellence abroad for the creation and application of surveillance techniques. Global outsourcing will therefore be successful if these capabilities are integrated and methods with a direct impact on risk management and risk communication are improved, in addition to reducing PV costs.
Proactive safety initiatives are planned.
Launching a product is an important step in the development of a drug because it signifies the conclusion of discussions between the pharmaceutical industry, regulatory agencies, and patients. As part of the new PV vision, stakeholders should be educated even before the commercial launch. Therefore, it would be possible to implement earlier close monitoring and education practices before the drug was released on the market with the help of conditional marketing authorizations. The patient safety advertisements will also improve and increase adverse event reporting. Furthermore, it would lead to the best possible use of the product and an improvement of the benefit-risk profile of the drug.
This would give PV the chance to raise awareness about safety concerns while also taking advantage of the chance to collect more thorough safety data during the early stages of the drug’s use. This strategy would produce a reasonable hybrid alternative by combining common safety surveillance techniques with the evaluation of post-marketing safety using sizable mortality and morbidity trials before the drug’s approval and introduction.
Reliability
Safety findings must be conveyed in a timely, clear, and concise manner for the new paradigm of an improved and proactive pharmacovigilance system to be successful. To guarantee that all available safety data are used in the risk assessment of potential signals, this will necessitate the development of a unified adverse event reporting system, including a storage database and analytical tool that would be shared by sponsors. Such a cross-company safety data tool could be made possible by recent technological developments, enabling more accurate background rate determination and signal detection.
A “Next generation PV” model’s development will be heavily influenced by current shifts in the cost and insurance coverage of new medications, the regulatory landscape, and the effects of global financial changes on the pharmaceutical industry. Pharmaceutical companies are being pushed harder than ever to reinvent themselves by speeding up development, being agile and efficient, addressing unmet medical needs that are already present, and enhancing patient value. To transform current systems into high-performing organizations with new signal detection technologies, emerging markets, world-class talent on safety assessment, and cost-efficiencies consistently integrated, PV departments will need to form cooperative partnerships with existing and new stakeholders. However, in order to implement these organizational changes, the company will need to change its corporate philosophy.
A career in drug safety and pharmacovigilance can be started by enrolling in Sollers College today.
Every step of the curriculum will help you with your PV skills. There are training programs available from Sollers college for students who are prepared to build their profiles.
You can increase your skill set with the help of Sollers college, who also offer lots of opportunities to do so. Achieve success in your career with in-demand certifications.
A variety of career options are consistently created by Sollers College’s distinctive curriculum, which also provides the best professional supervision and rapid learning support.
Sollers College built a path to the significant pharmaceutical industry so that you could learn and share your knowledge. Don’t limit your options to the pharmaceutical market!!!